he El Rio Special
Immunology Associates clinic is part of the El Rio Community Health
Center,
a large community health center in Tucson, Arizona, and provides primary
care (inpatient and
(outpatient) as well as consultative care to approximately 1500 persons living with HIV infection
in Southern Arizona. The staff includes four physicians, an adult nurse practitioner, a psychiatric
nurse practitioner, a substance abuse counselor, two social workers who provide individual and
group psychotherapy, a part-time dietician, and five continuity of care coordinators (3Cs). Funding
is via Medicaid (Arizona Healthcare Cost Containment System), Medicare, commercial insurance,
and Ryan White Title II, III, and Special Projects of National Significance (SPNS).
Our clinic currently has two SPNS projects: one is directed at developing comprehensive HIV care
for persons living along the Arizona- Mexico border and the other is a “prevention with positives”
program. The five 3Cs on the staff represent a unique and essential component to our efforts. They
are fundamentally the “jack-of-all-trades” staff that does whatever needs to be done to ensure no one
falls through the cracks of the system. This may entail eligibility assistance, coordinating with AIDS
service organizations or with other care systems, such as disability and mental health; delivering
medication boxes; and assisting with food, housing, and transportation. They also provide health
education, including supplemental medication adherence and secondary HIV prevention counseling.
Their final role is to provide an extra ear to hear patient concerns and problems that patients may not
bring to the attention of the physician.
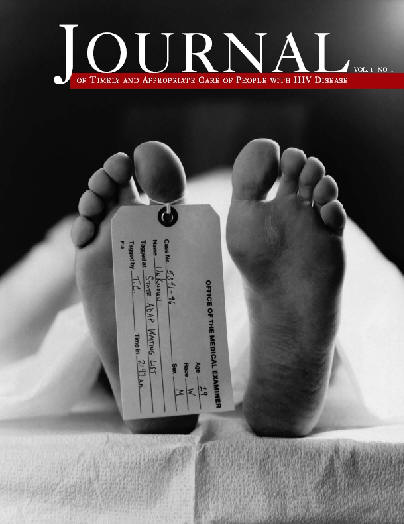
The role of the 3C is critical to the clinic’s success because we have found that keeping people with
HIV infection in care and adherent to medications is the key to keeping them alive and living meaningful
lives. In 1995, there were 76 deaths or 14 per 100 patient years. HIV protease inhibitors were approved by
the Federal Drug Administration in the beginning of 1996 and effective antiretroviral therapy then became
widely available. The death rate decreased by 50% during 1996, and in the years since, the mortality
rate has ranged from 2 to 4 deaths per 100 patient years. Nevertheless, a significant number of patients
are still dying. A review of the 30 patient deaths in 2002 found that 93% of those who died carried an AIDS
diagnosis.
Additionally 70% of those who died were not receiving antiretroviral therapy despite the lack of any financial
for administrative barrier to obtaining these medications during 2002. The causes of death were examined,
and substance abuse was found to be the leading cause of death (13 of the 30 deaths). Chronic infection
with Coccidioidomycosis, which is a fungal infection endemic to the Southwest, was the second most
common cause of death (7 of the 30 deaths). This infection is generally treatable but requires a high level
of adherence to antifungal medications and antiretroviral therapy. This analysis suggests that the major risk
factor of death among persons in our clinic is the presence of substance abuse and mental health issues
that prevent these persons from fully benefiting from antiretroviral and other therapies.
For this reason, quality HIV treatment requires a comprehensive range of services that will best enable
patients with these risk factors to start and stay on treatment. As we move toward Ryan White reauthorization,
we need to understand that our health care system is profoundly broken. Ryan White funding functions to fix
this system to serve the needs of persons living with HIV/AIDS. The first step in the reauthorization should be
to define and mandate core primary care services for persons living with HIV/AIDS.
However, let me be clear that simply providing access to antiretroviral therapy is inadequate. Patients need
to have access not only to antiretroviral drugs but also to support systems to ensure that they obtain maximum
benefit from treatment. Therefore, core primary care services need to include primary medical care that is
expert in the management of antiretroviral therapy and the treatment of opportunistic infection, mental
health care including access to psychiatric medications, substance abuse treatment, and continuity of care
coordination (to include secondary prevention and adherence). Second, we need to address the inequality and
inadequacy of the state AIDS Drug Assistance Programs (ADAPs). Inequalities exist both between and within
states. A minimum formulary that includes antiretroviral therapy, prophylaxis for opportunistic infections, and
required immunizations should be established and funded.
Additionally, the number of underinsured patients is increasing, and these patients are often not covered
by ADAP; legislation to fix this large hole in Medicare and commercial insurance plans should be included in
Ryan White legislation. Third, we need to make sure that the people living with HIV in rural communities have
access to the same range of services as those offered in urban areas. Finally, we need to develop more HIV
primary care expertise. Incentives are needed for HIV training programs and for primary care providers that care
for persons living with HIV.
Consultation mechanisms to share HIV expertise are needed for areas with relatively small at-risk or infected
populations. El Rio Special Immunology Associates is able to offer a comprehensive range of services and is a
reminder, despite hearing about all the present concerns and problems with funding, of what the end product
of Ryan White funding can be. We have endeavored to treat every patient with compassion and expertise, and
thus far, we have been able to honor this commitment.
Our challenge—and that of the Ryan White reauthorization process is to continue to be able to do so as
the number of persons living with HIV continues to increase and as their care becomes more complex.